The year is 1928. While inspecting a contaminated petri dish of Staphylococcus bacteria, British scientist Alexander Fleming makes a crucial observation: a growth of mold belonging to the Penicillium genus. Upon closer examination, he noticed a ring around the mold where the bacteria ceased to grow. As Fleming would later find out, this particular mold marked the advent of the world’s first antibiotic — penicillin. With its antimicrobial properties, penicillin can cure bacterial infections that once meant almost certain death, and it has transformed the medical industry by spurring the discovery of other antibiotics.
Over time, antibiotics have increased in variety and efficacy, earning them the title of “miracle drugs”. However, fast forward to 2024, and the efficacy of antibiotics is waning. The rise of antimicrobial resistance poses a serious threat to global health, as bacteria evolve and render these “miracle drugs” increasingly ineffective.
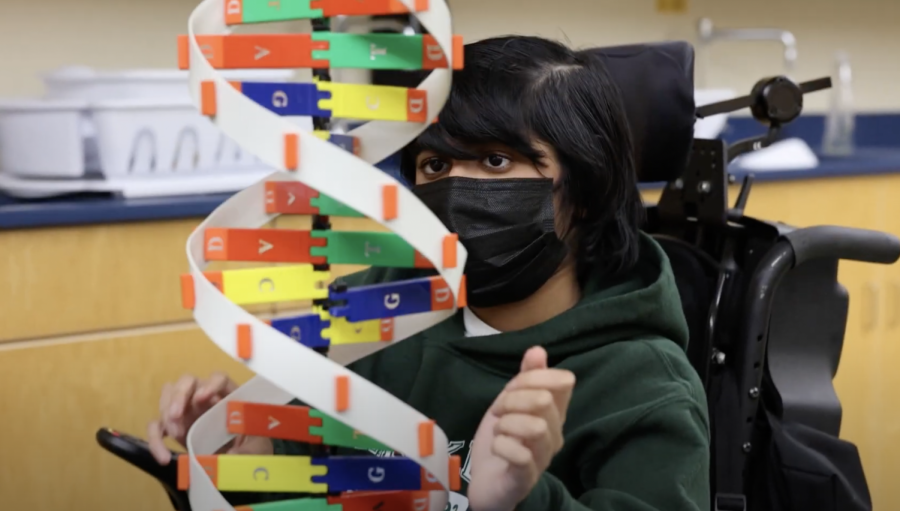
AMR occurs when microorganisms like bacteria develop resistance to antimicrobial agents. The most well-known antimicrobial agents are antibiotics, which are used to treat bacterial infections like the common cold, pneumonia and sepsis. Bacteria can acquire resistance genes from other bacteria through horizontal gene transfer methods like conjugation and transformation. In conjugation, circular DNA molecules called plasmids transfer genetic material between different bacteria. Transformation occurs when bacteria inherit genes from dead bacteria in the environment.
At its core, AMR is based on the natural selection and evolution of microorganisms. When exposed to an antibiotic, susceptible bacteria are eliminated, leaving behind a population of microorganisms with genes that are resistant to the antibiotic. After multiplying over successive generations, the resistant gene becomes dominant, and the species of bacteria no longer reacts to the antibiotic. Public Health Club adviser, biology YouTuber and upper school business teacher Patrick Kelly reflects on the pressing issue of AMR.
“There were a few decades from the 1940s through the 1960s where scientists developed tons of new antibiotics, and it seemed like humans had finally beat bacteria,” Kelly said. “These days, bacteria are developing resistance to our current crop of antibiotics faster than researchers and pharmaceutical companies can find new antibiotics.”
AMR persists as a pervasive yet often overlooked issue. Despite the World Health Organization’s recognition of AMR as one of the top ten global public health threats, there remains a lack of awareness about its significance. In a 2015 survey conducted across 12 countries by the WHO, 64% of respondents lacked a clear understanding of the impact of AMR on their lives and health.
In the past decade, the emergence of antibiotic-resistant bacteria strains in Escherichia coli, Salmonella and Staphylococcus aureus has become a global concern. In 2008, Methicillin-resistant Staphylococcus aureus colonization affected 32 infants and 13 family members in a neonatal intensive care unit in Denmark. In early 2019, an outbreak of antibiotic-resistant salmonella originating from Mexican food sources caused 255 infections and 60 hospitalizations. And in recent years, antibiotic-resistant E. coli in romaine lettuce has resulted in foodborne illnesses like gastroenteritis and food poisoning.
These cases represent only a fraction of the widespread instances of AMR occurring worldwide. More recently, a mysterious dog virus has spread across seven U.S. states, with some sources claiming that the illness does not respond to antibiotics or antivirals. Infected dogs exhibit excessive coughing and sneezing, and those with severe respiratory infections are at risk of developing pneumonia.
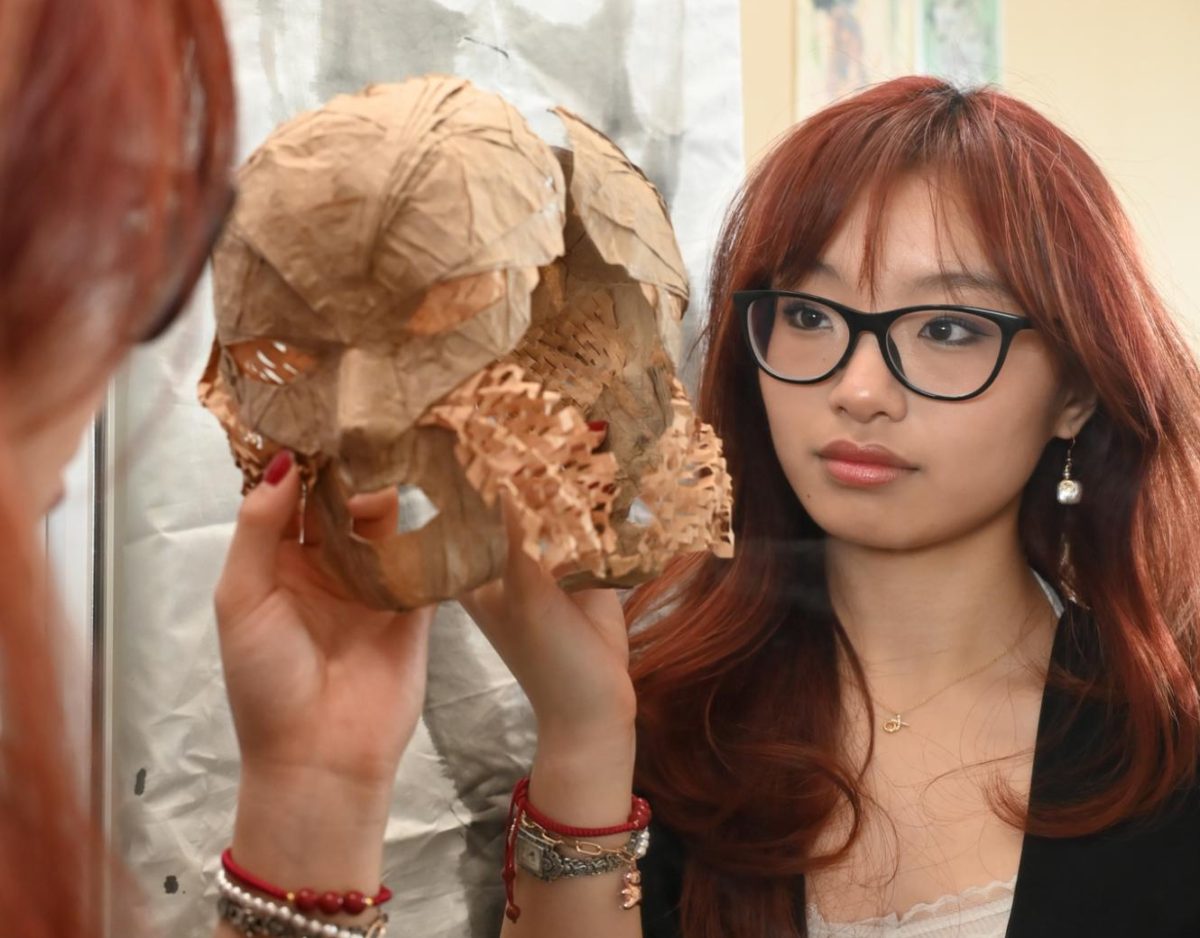
The common misuse of antimicrobial agents aggravates the problem of AMR. Overprescription of antibiotics and taking antibiotics for non-bacterial infections can lead to quicker and more effective development of resistant bacteria strains, to the point where the antimicrobials do not work against them anymore. For this reason, doctors often seek alternative solutions such as vaccines or probiotics before prescribing antibiotics as a last resort. Public Health Club president Fiona Yan (12) explains how widespread overprescription inflames AMR cases globally, a phenomenon she saw firsthand while living abroad.
“Antibiotic resistance is not only a science topic but also a cultural one,” Fiona said. “[In] a lot of countries around the world, the culture of the medical system promotes overprescription of antibiotics, which exacerbates resistance. Having lived in China, where overprescription is common, I am aware of the severity of [AMR].”
Nonetheless, there are ways to combat the spread of AMR. When prescribed with antibiotics, it is important to finish the entire prescription to avoid leaving behind the strongest, most resistant bacteria, which often develop resistant strains.
The widespread use of antibiotics in agriculture also accelerates the spread of resistant bacteria. Kelly advocates for the purchase of antibiotic-free foods.
“Use your dollar’s voting power and buy meat from farmers that don’t use antibiotics,” Kelly said. “By buying antibiotic-free chicken, you’re sending a message to the meat industry that will hopefully persuade them to cut back on antibiotics.”
It is crucial to recognize our collective capacity to combat AMR. Individual actions like adhering to proper antibiotic use, advocating for responsible agricultural practices or promoting public awareness ensures a healthier, AMR-free future for generations to come.
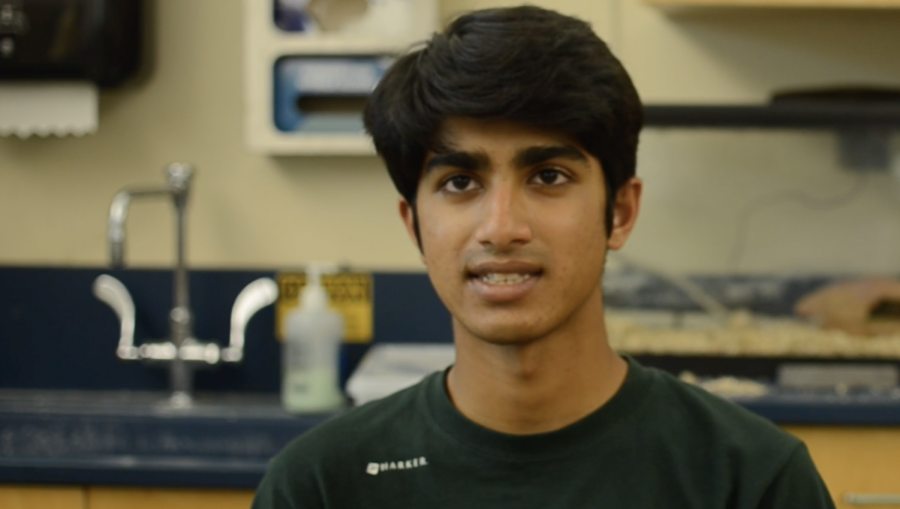
“Antibiotic resistance is a growing issue that threatens the ability to treat bacterial infections,” Medical Club officer Mindy Truong (10) said. “More research is needed to address the issue to find solutions beyond antibiotics, and hopefully, sustainable solutions can be achieved through education and awareness about this issue.”















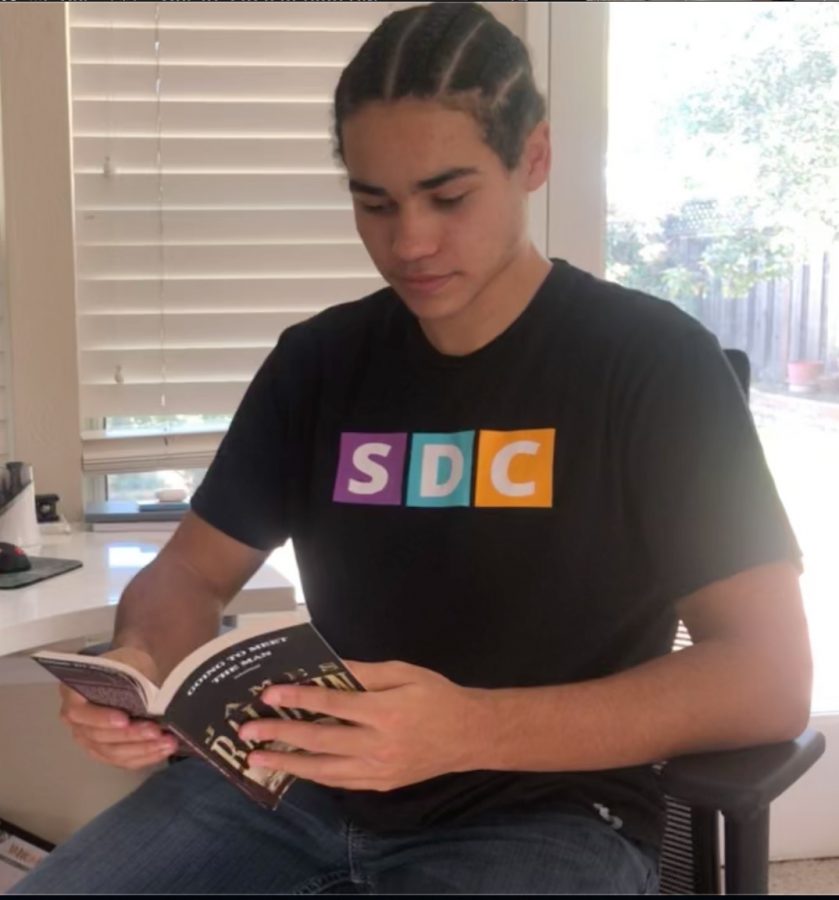
![“[Building nerf blasters] became this outlet of creativity for me that hasn't been matched by anything else. The process [of] making a build complete to your desire is such a painstakingly difficult process, but I've had to learn from [the skills needed from] soldering to proper painting. There's so many different options for everything, if you think about it, it exists. The best part is [that] if it doesn't exist, you can build it yourself," Ishaan Parate said.](https://harkeraquila.com/wp-content/uploads/2022/08/DSC_8149-900x604.jpg)



![“When I came into high school, I was ready to be a follower. But DECA was a game changer for me. It helped me overcome my fear of public speaking, and it's played such a major role in who I've become today. To be able to successfully lead a chapter of 150 students, an officer team and be one of the upperclassmen I once really admired is something I'm [really] proud of,” Anvitha Tummala ('21) said.](https://harkeraquila.com/wp-content/uploads/2021/07/Screen-Shot-2021-07-25-at-9.50.05-AM-900x594.png)





![“I think getting up in the morning and having a sense of purpose [is exciting]. I think without a certain amount of drive, life is kind of obsolete and mundane, and I think having that every single day is what makes each day unique and kind of makes life exciting,” Neymika Jain (12) said.](https://harkeraquila.com/wp-content/uploads/2017/06/Screen-Shot-2017-06-03-at-4.54.16-PM.png)








![“My slogan is ‘slow feet, don’t eat, and I’m hungry.’ You need to run fast to get where you are–you aren't going to get those championships if you aren't fast,” Angel Cervantes (12) said. “I want to do well in school on my tests and in track and win championships for my team. I live by that, [and] I can do that anywhere: in the classroom or on the field.”](https://harkeraquila.com/wp-content/uploads/2018/06/DSC5146-900x601.jpg)
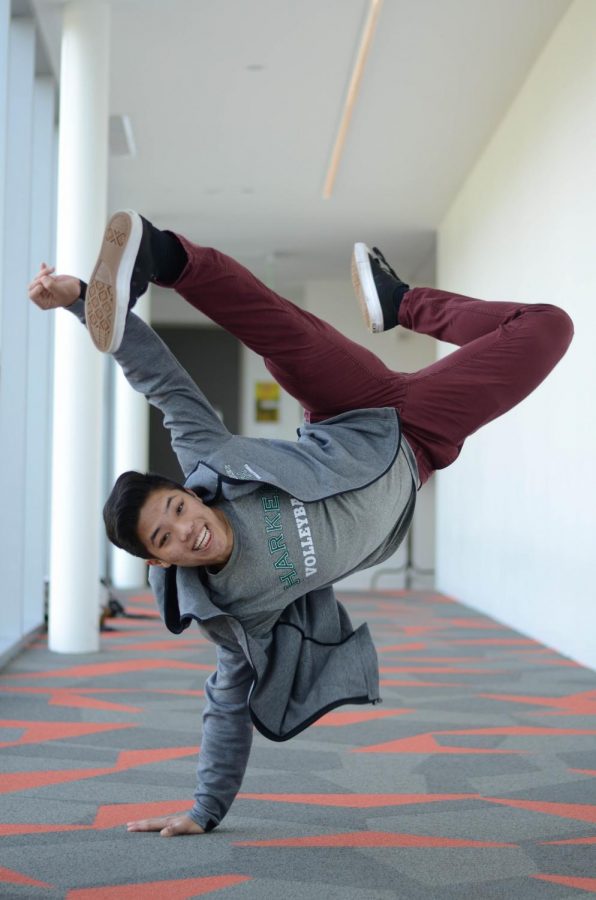
![“[Volleyball has] taught me how to fall correctly, and another thing it taught is that you don’t have to be the best at something to be good at it. If you just hit the ball in a smart way, then it still scores points and you’re good at it. You could be a background player and still make a much bigger impact on the team than you would think,” Anya Gert (’20) said.](https://harkeraquila.com/wp-content/uploads/2020/06/AnnaGert_JinTuan_HoHPhotoEdited-600x900.jpeg)
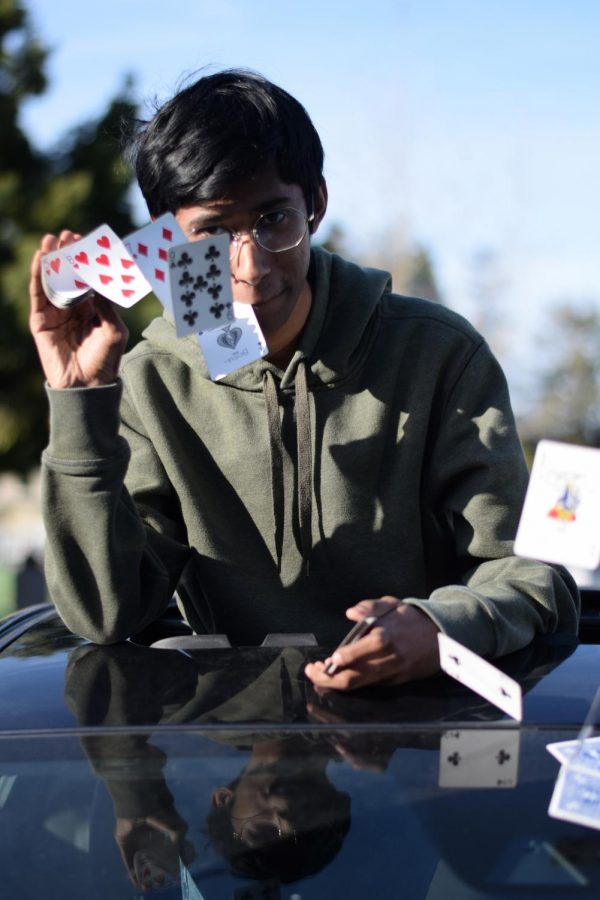
![“I'm not nearly there yet, but [my confidence has] definitely been getting better since I was pretty shy and timid coming into Harker my freshman year. I know that there's a lot of people that are really confident in what they do, and I really admire them. Everyone's so driven and that has really pushed me to kind of try to find my own place in high school and be more confident,” Alyssa Huang (’20) said.](https://harkeraquila.com/wp-content/uploads/2020/06/AlyssaHuang_EmilyChen_HoHPhoto-900x749.jpeg)