As we slog through another respiratory virus season, COVID-19 is no longer the main topic of discussion. Instead, the nation seems to have collectively moved on, despite the dangers the virus still poses. So what’s new with COVID-19? And should we be more cautious?
COVID-19 continues to mutate into new variants like the most recent JN.1 strain and remains especially active during the respiratory virus season from fall to winter. Updated vaccines by Pfizer-BioNTech, Moderna, and Novavax that came out in fall 2023 are effective against newer variants, and CDC safety precautions have largely stayed the same since last year. Biology teacher Mike Pistacchi commented on the changing attitudes toward COVID-19.
“It’s still problematic in the sense that hospitalizations are up,” Pistacchi said. “People do die from COVID-19. Is it a problem to the point where we need to keep living differently because of it? That’s starting to come down more to personal opinion. Which precautions you take are largely gonna be biased by your personal health situation and your family health situation.”
The California Department of Public Health removed the standard five-day isolation period from its COVID-19 guidelines early this January, shifting to symptom-based quarantine after the first 24 hours of infection. While COVID-19’s presence at the upper school has remained low relative to the past two years, nurse Jennifer Olson noted the implications of this new policy.
“The new guidelines blend what we normally had pre-COVID for any sort of respiratory virus with the measures that came with COVID,” Olson said. “But it’s an interesting time for the guidance to change now as far as the seasons go. So I think while we all suspected this would happen, maybe we didn’t expect it [to happen] this soon.”
Since the COVID-19 public health emergency ended in May 2023, test kits and medicines have transitioned to the commercial market. Paxlovid, an at-home oral medication that treats high-risk COVID cases in adults, started accepting commercial orders last November at nearly $1,400 per treatment course, triple the price at which it was sold to the U.S. government.
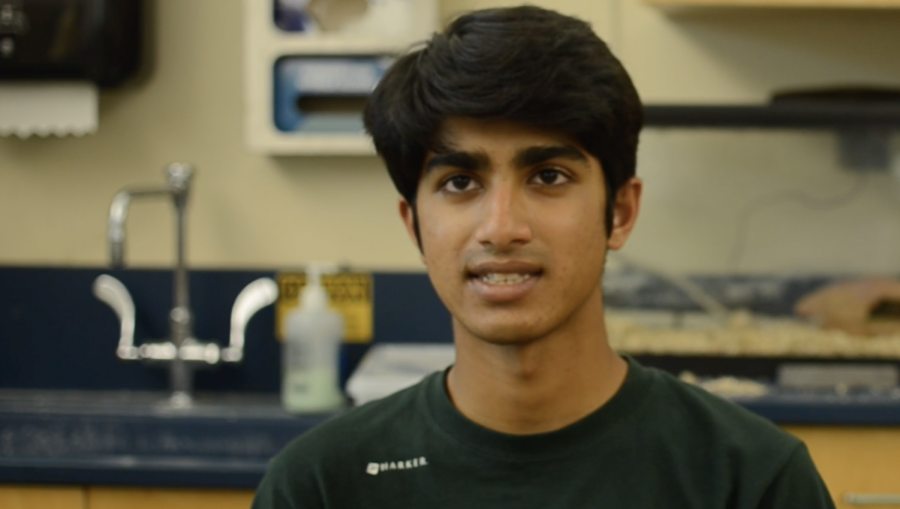
Consumers will need to rely on their own insurance to access COVID-19 resources once federal stockpiles run out. Harker Public Health Club co-president Fiona Yan (12) believes that diminishing access to these tools may discourage the public from maintaining proper precautions against disease.
“A lot of these things aren’t free anymore, which could be part of the reason why less people are getting treatment and taking measures to prevent the disease,” Fiona said. “People also aren’t taking things like new variants as seriously because they come back every year now, and everyone’s tired of them. But that could change the way and extent to which COVID spreads.”
COVID-19 cases in San Jose exceed their levels from a year ago in January 2022, but the impact of the virus fluctuates with more than just the number of cases. Physics and research teacher Chris Spenner discussed why recent COVID-19 variants have evolved to become less deadly than the original strain.
“From an evolutionary standpoint, there’s an advantage for the virus to become less deadly,” Spenner said. “Killing off the host doesn’t help the virus. It just needs to be able to transmit and then it’s done with the host. It has become less deadly, but that is somewhat illusory because to some degree, it has already killed off so many people who were susceptible.”
Scientists continue to discover new aspects of COVID-19, including a phenomenon called long COVID, which inflicts people with symptoms like fatigue, fever and difficulty sleeping for months or even years after they recover from the original virus. A recent study suggests that in patients with long COVID, part of the immune system remains active after the virus dies, leading to persistent symptoms. Pistacchi shared his thoughts on long COVID and other long viral diseases.
“It’s certainly real, and we’re learning a lot about what viruses do with your body,” Pistacchi said. “There are also, however, long versions of many viral diseases. And we’ve largely ignored that until COVID hit so many people so hard. We tend to ignore things like long flu in people who already have health problems: coronavirus landed on a lot of healthy people who are now saying, two years later, they still have these problems. Now it’s caught our attention.”
People who are not vaccinated, have severe COVID-19 or have other health issues are more at risk of long COVID. Spenner hopes that a better understanding of COVID-19 will allow more people to make healthy decisions.
“I wish that we had a lot more discussions publicly, both as a school and a society, about good practices for watching out for each other,” Spenner said. “Because when the public health is not doing well, that puts us and people who we care about at risk. So we have a selfish interest in watching out for other people’s health and tracking and correcting behaviors, especially at a school. It’s all about education.”















![“[Building nerf blasters] became this outlet of creativity for me that hasn't been matched by anything else. The process [of] making a build complete to your desire is such a painstakingly difficult process, but I've had to learn from [the skills needed from] soldering to proper painting. There's so many different options for everything, if you think about it, it exists. The best part is [that] if it doesn't exist, you can build it yourself," Ishaan Parate said.](https://harkeraquila.com/wp-content/uploads/2022/08/DSC_8149-900x604.jpg)



![“When I came into high school, I was ready to be a follower. But DECA was a game changer for me. It helped me overcome my fear of public speaking, and it's played such a major role in who I've become today. To be able to successfully lead a chapter of 150 students, an officer team and be one of the upperclassmen I once really admired is something I'm [really] proud of,” Anvitha Tummala ('21) said.](https://harkeraquila.com/wp-content/uploads/2021/07/Screen-Shot-2021-07-25-at-9.50.05-AM-900x594.png)





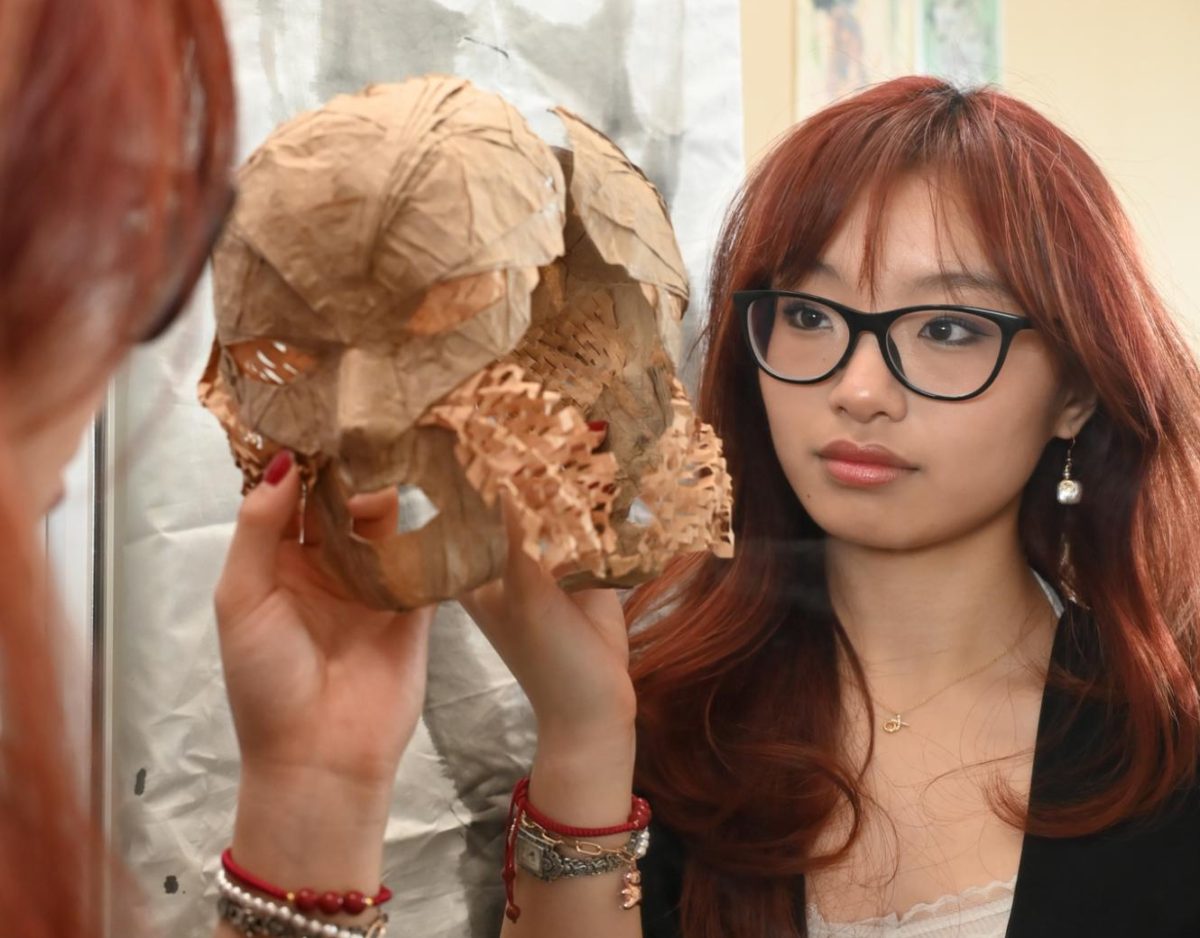
![“I think getting up in the morning and having a sense of purpose [is exciting]. I think without a certain amount of drive, life is kind of obsolete and mundane, and I think having that every single day is what makes each day unique and kind of makes life exciting,” Neymika Jain (12) said.](https://harkeraquila.com/wp-content/uploads/2017/06/Screen-Shot-2017-06-03-at-4.54.16-PM.png)








![“My slogan is ‘slow feet, don’t eat, and I’m hungry.’ You need to run fast to get where you are–you aren't going to get those championships if you aren't fast,” Angel Cervantes (12) said. “I want to do well in school on my tests and in track and win championships for my team. I live by that, [and] I can do that anywhere: in the classroom or on the field.”](https://harkeraquila.com/wp-content/uploads/2018/06/DSC5146-900x601.jpg)
![“[Volleyball has] taught me how to fall correctly, and another thing it taught is that you don’t have to be the best at something to be good at it. If you just hit the ball in a smart way, then it still scores points and you’re good at it. You could be a background player and still make a much bigger impact on the team than you would think,” Anya Gert (’20) said.](https://harkeraquila.com/wp-content/uploads/2020/06/AnnaGert_JinTuan_HoHPhotoEdited-600x900.jpeg)
![“I'm not nearly there yet, but [my confidence has] definitely been getting better since I was pretty shy and timid coming into Harker my freshman year. I know that there's a lot of people that are really confident in what they do, and I really admire them. Everyone's so driven and that has really pushed me to kind of try to find my own place in high school and be more confident,” Alyssa Huang (’20) said.](https://harkeraquila.com/wp-content/uploads/2020/06/AlyssaHuang_EmilyChen_HoHPhoto-900x749.jpeg)